Introduction
- Serious chronic skin disease
- Pemphigus derived from Greek word pemphix meaning bubble or blister
- Characterized by appearance of vesicles and bullae that develop in cycles
Definition
- Pemphigus includes a group of autoimmune blistering diseases of the skin and mucous membranes characterized histologically by intradermal blisters and immunologically by the finding of circulating immunoglobulin G (IgG) antibody directed against the cell surface of keratinocytes.
Types
- 1 -Pemphigus Vulgaris (Most Common, 70% cases)
- 2 - Pemphigus Foliaceus
- 3 - Paraneoplastic Pemphigus
Pemphigus Vulgaris
- Pemphigus vulgaris (PV) is an autoimmune, intraepithelial, blistering disease affecting the skin and mucous membranes and is mediated by circulating autoantibodies directed against keratinocyte cell surfaces.
Etiology
- Blisters in PV are associated with the binding of IgG autoantibodies to keratinocyte cell surface molecules.
- These intercellular or PV antibodies bind to keratinocyte desmosomes and to desmosome free areas of the keratinocyte cell membrane.
- The binding of autoantibodies results in a loss of cell-cell adhesion i.e. cell separation
- Pemphigus antibody binds to keratinocyte cell surface molecules desmoglein 1 and desmoglein 3.
- Patients with the active disease have circulating and tissue-bound autoantibodies of both the immunoglobulin G1 and G4 subclasses.
Clinical Features
- Equal gender predilection
- mean age: 50 -60 years
- characterized by rapid appearance of vesicles and bullae, varying in diameter from a few mm to several cm
- large areas of the skin surface may be covered
- These lesions contain a thin, watery fluid shortly after development, but this may soon become purulent or sanguineous.
- When bullae rupture, they leave a raw eroded surface
- Nikolsky's sign - when focal areas of epithelium slide off either under oblique pressure or spontaneously without the prior formation of a vesicle or bulla. The loss of epithelium occasioned by rubbing apparently unaffected skin is termed Nikolsky's sign. It is a characteristic feature of pemphigus and is caused by prevesicular edema which disrupts the dermal-epidermal junction.
- The course of pemphigus vulgaris is a variable.
Oral Manifestations
- Mucous membranes typically are affected first in PV.
- Mucosal lesions may precede cutaneous lesions by months.
- Disease involves mucosa in 50–70% of patients.
- Intact bullae are rare in the mouth.
- More commonly, patients have ill-defined, irregularly shaped, gingival, buccal or palatine erosions, which are painful and slow to heal
- The erosions extend peripherally with shedding of the epithelium.
- Erosions may be seen on any part of the oral cavity and can be scattered and often extensive.
- Erosions may spread to involve the larynx with subsequent hoarseness.
- Patient often unable to eat or drink adequately because the lesions are so uncomfortable.
- Other mucosal surfaces may be involved, including the conjunctiva, esophagus, labia, vagina, cervix, penis, urethra, and anus.
- Oral lesions are similar to those occurring on the skin.
Histopathological Features
- Characterized microscopically by the formation of a vesicle or bulla entirely intraepithelially, just above the basal layer producing the distinctive suprabasilar ‘split’
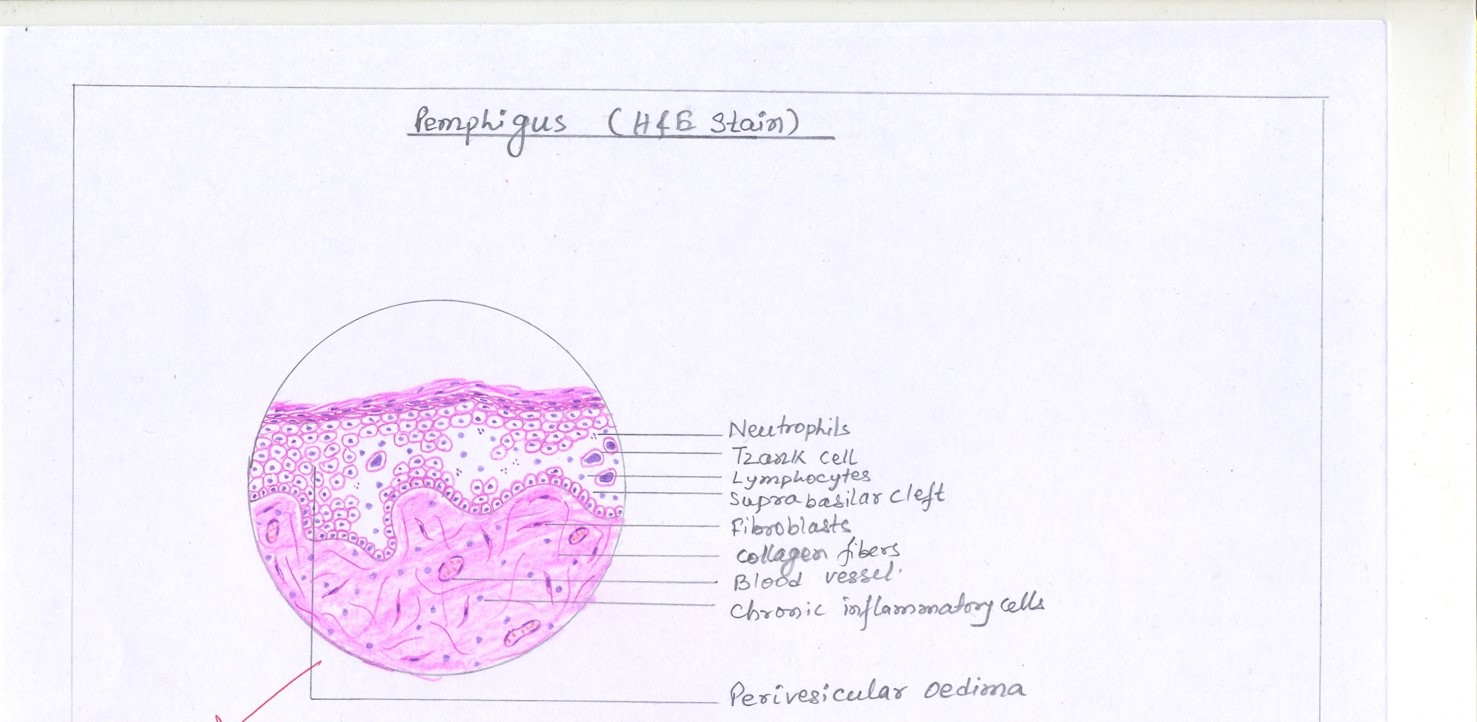
- Prevesicular edema appears to weaken this junction, and the intercellular bridges between the epithelial cells disappear. This results in loss of cohesiveness or acantholysis, and because of this, clumps of epithelial cells are often found lying free within the vesicular space. These have been called ‘Tzanck cells’
- Tzanck cells - degenerative changes which include swelling of the nuclei and hyperchromatic staining.
- Tzanck cells seen particularly in cytologic smears taken from early, freshly opened vesicles. Such smears form the basis for a rapid supplemental test for pemphigus, the ‘Tzanck test’
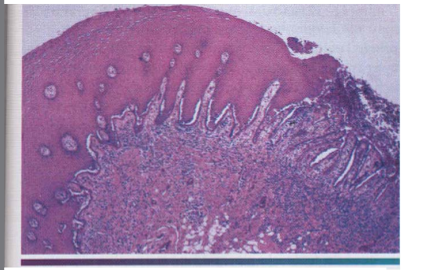
- Pemphigus Vulgaris - Low power View showing intra epithelial cleft just above basal cell layer
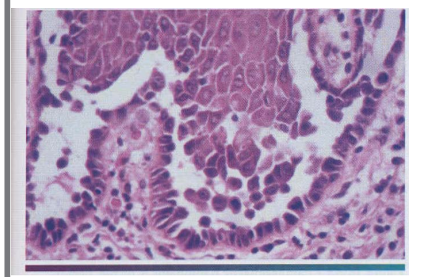
- Pemphigus Vulgaris - High power View showing round acantholytic epithelial cells within intra epithelial cleft
Differential Diagnosis
- dermatitis herpetiformis
- erythema multiforme bullosum
- bullous lichen planus
- epidermolysis bullosa
- bullous pemphigoid
- cicatricial pemphigoid
Treatment
- Aim of treatment in PV is the same as in other autoimmune bullous diseases, i.e. to decrease blister formation, promote healing of blisters and erosions, and determine the minimal dose of medication necessary to control the disease process.
- Corticosteroids
- There Are Potential Complications Of Long Term Use Of Systemic Corticosteroids
- PV Rarely Undergoes Complete Resolution
PEMPHIGUS FOLIACEOUS
- Autoimmune Skin Disorder
- Characterized By The Loss Of Intercellular Adhesion Of Keratinocytes In The Upper Parts Of The Epidermis (Acantholysis), Resulting In The Formation Of Superficial Blisters.
- Nikolsky Sign positive
- Chronic Course
- Little Or No Involvement Of The Mucous Membranes.
- Superficial blisters in PF are induced by immunoglobulin G (IgG) (mainly IgG4 subclass) autoantibodies directed against a cell adhesion molecule, desmoglein 1, expressed mainly in the granular layer of the epidermis.
- Characteristic Early Bullous Lesions Which Rapidly Rupture And Dry To Leave Masses Of Flakes Or Scales
- Relatively Mild Form Of Pemphigus
- Most Common In Older Adults
- H/F -Begins As Acantholysis Of The Upper Epidermis
- T/t is less aggressive than that for pemphigus vulgaris because of their lower morbidity and mortality rates.
Paraneoplastic Pemphigus
- Patients with underlying neoplasms who developed oral erosions and bullous skin eruptions
- all patients with paraneoplastic pemphigus have had tumors, most of which have been malignant.
- Most common malignancy associated with paraneoplastic pemphigus is non-Hodgkin lymphoma. Other associated malignancies include chronic lymphocytic leukemia, Castleman tumor etc.


