After reading this post you will learn the following about Oral Leukoplakia
- Introduction & Definition
- Etiology
- Clinical Features
- Histopathologic Features
- Diagnostic Procedures
- Treatment
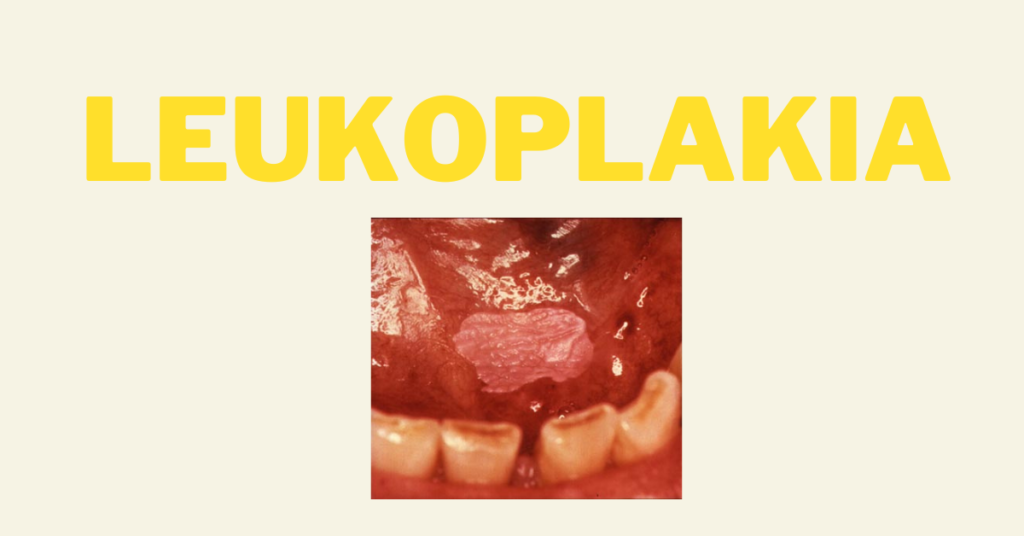
INTRODUCTION
- Also Known As Leukokeratosis
- Leukoplakia:-
- Leuko means White
- Plakia means Patch, Thus It’s A White Patch/Plaque In The Oral Cavity

- It’s a Premalignant Lesion/Potentially Malignant Disorder
- It’s the most common premalignant lesion/ most common potentially malignant disorder
- Various Studies Have Shown 0.6 To 20% Rate Of Malignant Transformation Of Leukoplakia
- Diagnosis Based On Exclusion Of Other Lesions Which Present As Oral White Plaques. Examples Of Other White Lesions Are:-
- Hypertrophic Lichen Planus
- Chronic Cheek Bite
- Frictional Keratosis
- Tobacco Induced Keratosis Leukoedema
- White Sponge Nevus
DEFINITION A Predominantly White Lesion Of The Oral Mucosa That Cannot Be Characterized As Any Other Definable Lesion; Some Oral Leukoplakia Will Transform Into Cancer” (Axell T, 1996)
- Clinical Term Indicating A White Patch Or Plaque Of Oral Mucosa
- Cannot Be Rubbed Off
- Cannot Be Characterized Clinically As Any Other Disease
- Biopsy Is Mandatory To Establish A Definitive Diagnosis
- When Biopsy Taken The Term Leukoplakia Replaced By Diagnosis Obtained Histologically
- Localized In Distribution (Lesion)
- Hyperkeratotic (Increased Keratin Production)
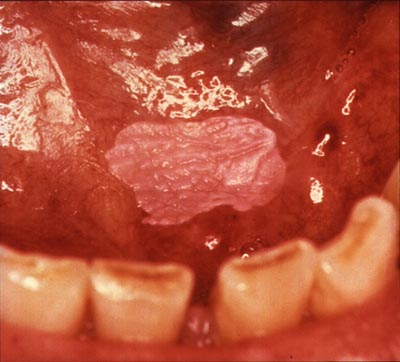
- White In Appearance Due To Wetting Of Keratotic Patch While In Contact With Saliva Or Thickened Spinous Layer Which Masks Vascularity Of Underlying Connective tissue
- Leukoplakia Is An Adaptive Response Of Viable Healthy Oral Mucosa To Sustained Low Grade Irritation:-
- Mechanical
- Chemical
- Galvanic
- Diagnosis of Leukoplakia Denotes That The Mucosa Is Trying To Adapt To The Noxious Stimuli By Undergoing Hyperkeratinization Of Its Surface (Example Of Tissue Adaptation)
ETIOLOGY
- Tobacco

- Tobacco smoking Is Most Closely Associated With Leukoplakia
- More Common In Smokers Than Non Smokers
- Reducing or Cessation Of Tobacco May Result In Regression Or Disappearance Of Oral Leukoplakia

- Other Factors May Have A Role In Etiology. Such As:-
- Alcohol Abuse – Alcohol Exerts A Strong Synergistic Effect With Tobacco In Oral Cancer Development. Nevertheless, There Is Conflicting Evidence As To Whether Alcohol Is Associated Independently With Leukoplakia
- C. Albicans Infection
- Chronic Trauma
- Sanguinaria (Persons Using Toothpaste Or Mouth Rinses Containing Herbal Extract, Sanguinaria)
- UV Rays – Leukoplakia Of Lower Lip Vermilion
- HPV Strains Like 16,18 – Uncertain
- Genetic Factors – Little Known
- Nutritional Factors Have Been Cited As Important, Especially Iron Deficiency Anemia
CLINICAL FEATURES
- AGE:-
- Middle Age To Older Individuals
- Peak Incidence Above 50 Years
- GENDER PREDILECTION :-
- Varies In Different Studies
- Strong Male Predilection In India
- 1:1 i.e. Equal Predilection In Western World
- SITE OF OCCURRENCE:-
- Buccal Mucosa
- Gingiva
- Lip Vermillion
- Tongue
- Floor Of Mouth
- COLOR:- Generally Seen As Grey, White Or Yellowish White In Color
- CLINICAL APPEARANCE:- Leukoplakia Presents A Diverse Clinical Appearance And With Time Its Appearance Often Changes:-
- Preleukoplakia – A Low-grade Or Very Mild Reaction Of The Oral Mucosa, Appearing As A Grey Or Greyish-white, But Never Completely White Area With A Slightly Lobular Pattern And With Indistinct Borders Blending Into The Adjacent Normal Mucosa (Pindborg Et Al, 1968).
- Mild Or Thin Leukoplakia – Characteristically Soft And Flat And Is Sometimes Wrinkled Or Fissured. Borders Usually Sharply Demarcated (Rarely Shows Dysplasia)
- Thick Or Homogeneous Leukoplakia – Later, The Lesions Become Thicker, Extend Laterally And Become More Whitish In Color. The Fissures May Become Deepen And Leathery On Palpation. On Palpation, It May Feel Leathery, Dry, Or Like Cracked Mud.
- Granular Or Nodular Leukoplakia – Some Severe Lesions Develop Surface Irregularities And Are Designated As Granular Or Nodular Leukoplakia.
- Verrucous Leukoplakia – Show Sharp Or Blunt Projections

- Erythroleukoplakia/Speckled Leukoplakia Or Non Homogeneous Leukoplakia – Mixed Red And White Lesions Are Designated As Erythroleukoplakia, Speckled Leukoplakia Or Non Homogeneous Leukoplakia. These Lesions Have Been Shown To Have A Higher Malignant Transformation Rates.

LEUKOPLAKIA – CLINICAL CLASSIFICATION:-
WHO in 1980 Recommended subdivisions to record various clinical forms of leukoplakia:-
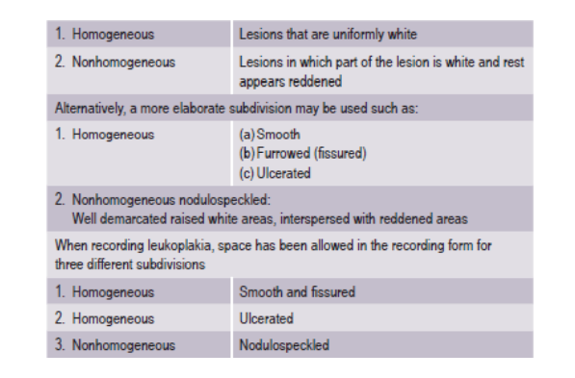
- Homogeneous – Asymptomatic and show a very low risk of malignant transformation
- Non Homogeneous – Pain, itching and discomfort. These show a high risk for malignant transformation
- Proliferative Verrucous Leukoplakia (PVL):–
- PVL Is An Aggressive Variant Of Leukoplakia
- Common In Females
- Minimal Association With Tobacco Use
- From Single Lesion It Progresses To Multiple Lesions
- Characterized By Development Of Multiple, Slowly Spreading, Keratotic Plaques With Rough Surface Projections
- Lesions Rarely Regress Despite Therapy
- Recurrence After Treatment
- A Strong Potential For Malignant Transformation
- Diagnosis Often Made Late In The Protracted Course Of PVL With The Disease In An Advanced Stage When It Is Especially Refractory To Treatment
HISTOPATHOLOGIC FEATURES
- HALLMARK Of H/F Of Leukoplakia Are :-
- Epithelial Hyperplasia
- Surface Hyperkeratosis (Hyperparakeratosis Or Hyperorthokeratosis)
- Epithelial Dysplasia, If Present, May Range From Mild To Severe. In Some Instances, Carcinoma In Situ And Even Squamous Cell Carcinoma Are Encountered Histologically.
Histopathology Report Of Leukoplakia Should Always Include Statement Of Presence Or Absence Of Epithelial Dysplasia & An Assessment Of Its Severity
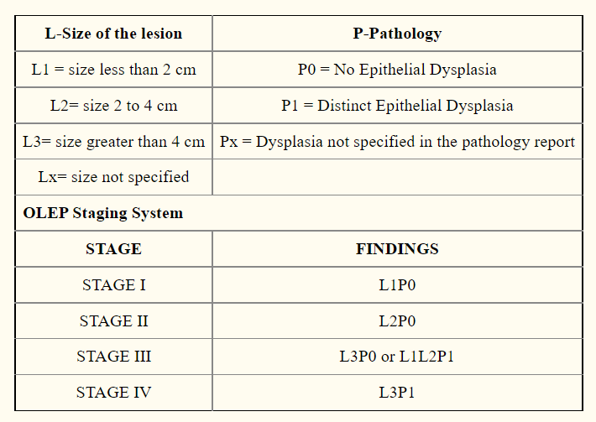
MODIFIED CLASSIFICATION AND STAGING SYSTEM FOR ORAL LEUKOPLAKIA (OLEP)[Van der Waal et al, 2000]
- It is Based on:–
- Size of lesion
- Presence or absence of epithelial dysplasia
- Altogether four stages are recognized:-
DIAGNOSTIC PROCEDURES:-
- Elimination Of Possible Causes –
- Rule Out Other Definable White Lesions Before Giving Clinical Diagnosis Of Oral Leukoplakia
- Biopsy-
- In Homogeneous Leukoplakia – Chances Of Epithelial Dysplasia & Malignant Transformation Low. But In Few Cases It Can Be Otherwise. Therefore Taking Biopsy Should Be A Standard Rule.
- Non Homogeneous Leukoplakia – Biopsy Taken At Site Of Symptoms If Present And /Or Site Of Redness/Induration.
- Diagnostic Methods Like Toluidine Blue & Exfoliative Cytology Are Of Limited Value In Leukoplakia.
TREATMENT
- Treat the cause (For example – Counselling the patient to stop habits like tobacco/alcohol is the primary step in the management of leukoplakia)
- The treatment may be conservative or surgical
- Surgical Excision (most common & treatment of choice)
- Other Treatment Modalities:-
- CO2 Laser Surgery
- Cryosurgery (liquid nitrogen)
- Retinoids & Other drugs
- Photodynamic Therapy
- Patients Follow-up Recommended
REFERENCES
- Shafer’s Textbook Of Oral Pathology
- Neville – Oral & Maxillofacial Pathology
- G Kiran et al. Leukoplakia – Review of A Potentially Malignant Disorder. J of Clinical & Diagnostic Research 2014; 8(8)
- Image – Wikipedia, Pixabay