After reading this post you will learn the following about Lichen Planus
- INTRODUCTION (GENERAL FEATURES)
- WHY CALLED AS LICHEN PLANUS
- ETIOLOGY
- CLINICAL FEATURES
- ORAL MANIFESTATIONS
- HISTOPATHOLOGIC FEATURES
- DIFFERENTIAL DIAGNOSIS
- MALIGNANT POTENTIAL
- TREATMENT
INTRODUCTION
- Oral Lichen Planus (OLP) Is a Common Mucocutaneous Disease
- First Described By Wilson In 1869
- Autoimmume
- Chronic
- Can Affect Either The Skin Or Mucosa Or Both
- It Can Cause Bilateral White Striations, Papules, Or Plaques On The Buccal Mucosa, Tongue, And Gingiva
- The Involvement Of The Oral Mucous Membrane Is So Frequent And Accompanies Or Precedes The Appearance Of Lesions On The Skin And Genital Mucous Membrane
- Affects 0.5-1% Of Worlds Population
WHY CALLED AS LICHEN PLANUS???
LICHENS Are Primitive Plants That Consists Of Symbiotic Algae & Fungi Growing On Solid Surfaces Like Bark Of Trees And Rocks.
PLANUS In Latin Means Flat


As The Condition Appears Similar To Lichen Found Growing On Trees And Rocks In Forests & The Skin Lesions Are Often Flat-topped And Can Be Somewhat Scaly, Hence The Name “LICHEN PLANUS”
ETIOLOGY
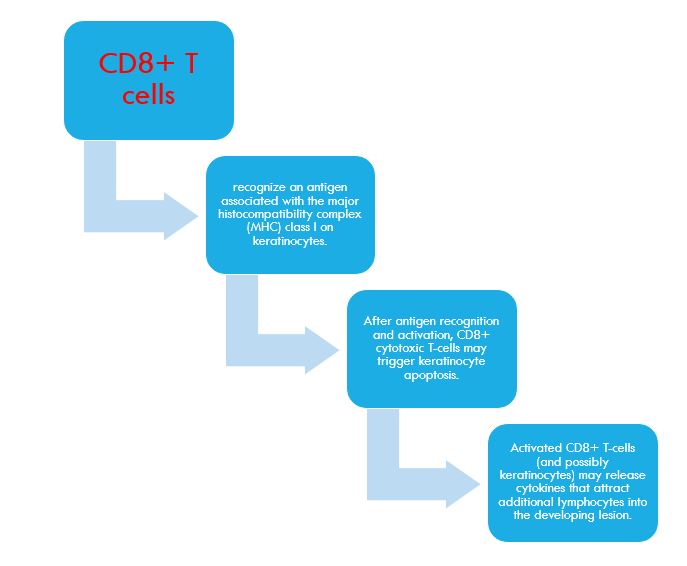
- Oral lichen planus is a T-cell-mediated autoimmune disease in which cytotoxic CD8+ T-cells trigger the apoptosis of oral epithelial cells.
- The precise cause of OLP is unknown. The lichen planus antigen is unknown, although it may be a self-peptide.
- PRECIPITATING FACTORS – The expression or unmasking of the lichen planus antigen may be induced by:-
- Drugs (lichenoid drug reaction), NSAIDS, Antimalarial Drugs
- Contact allergens in dental restorative materials or toothpastes (contact hypersensitivity reaction)
- Mechanical trauma where new lesions develop along the line of trauma (Koebner phenomenon)
- Viral infection
- Unidentified agents
- Rare in Carefree people, Common in Nervous, high-strung person

Interesting fact – Common in Nervous, high-strung person
- Course of the disease is long, from months to several years.
- Frequently undergoing periods of remission followed by exacerbations which often correspond to periods of emotional upset, overwork, anxiety or some form of mental strain. Other causes include traumatism (since outbreaks often develop along scratch lines), malnutrition and infection.
- GRINSPAN’S SYNDROME – An interesting association of lichen planus, diabetes mellitus & vascular hypertension.
CLINICAL FEATURES
- Oral lichen planus affects all racial groups
- SEX – Female-to-male ratio of 1.4:1
- AGE – adults older than 40 years, although younger adults and children can be affected.
Mnemonic To Remember Clinical Appearance of Skin lesions:-PPPPW - polygonal - papules - Purple - Pruritic (Itchy) - Wickham's striae (overlying, reticulated, fine greyish white lines)


- The lesions may occur anywhere on the skin surface, but usually are distributed in a bilaterally symmetrical pattern, most often on:
- flexor surfaces of the wrist and forearms
- inner aspect of the knees and thigh
- trunk, especially the sacral area
- The face frequently remains uninvolved.
- In chronic cases, hypertrophic plaques may develop, especially over the shins.
- The primary symptom of lichen planus is a severe pruritus (itching) that may be intolerable.
- In patients with OLP, scalp involvement (lichen planopilaris) and nail involvement is rare.
ORAL MANIFESTATIONS
- Majority of patients with dermal lichen planus have associated oral lesions of the disease
- In oral cavity, the disease assumes a somewhat different clinical appearance than on the skin
- RETICULAR FORM
- Classic & most common
- Lesions consisting of radiating white or gray, velvety, thread-like papules in a linear, annular or retiform arrangement forming typical lacy, reticular patches, rings and streaks over the buccal mucosa and to a lesser extent on the lips, tongue and palate.
- Greyish white glistening fine lines called as Wickham’s Striae
- A tiny white elevated dot is frequently present at the intersection of the Striae of Wickham
- When plaque-like lesions occur, radiating striae may often be seen on their periphery
- No significant symptoms, sometimes burning sensation may be present

- BULLOUS FORM
- Vesicle and bulla formation has been reported in oral lesions of lichen planus, but this is not a common finding ,difficult to diagnose
- When vesicles rupture it may clinically resemble erosive lichen planus
- EROSIVE FORM
- Erosions/ulcerative
- Begins as such and not as a progressive process from ‘nonerosive’ lichen planus
- Eroded or frankly ulcerated lesions are irregular in size and shape and appear as raw, painful areas
- Characteristic radiating striae may often be noted on the periphery of the individual lesions.
- Diagnosis possible if typical radiating striae & erythematous mucosa at periphery of ulcer
- Symptomatic

- ATROPHIC FORM
- Erythematous (Mucosal atrophy & red patches)
- appears clinically as smooth, red, poorly defined areas, often but not always with peripheral striae evident.
- Symptomatic
- Desquamative gingivitis
- red, diffuse, painful condition of the gingiva.
- It is now generally accepted that this is not an entity but represents a variety of conditions including the oral manifestations of several dermatologic diseases, one of which is lichen planus (usually the atrophic or erosive form), occurring on the gingiva
- Desquamative gingivitis
- HYPERTROPHIC FORM
- well-circumscribed, elevated white lesion resembling leukoplakia
- In such cases biopsy is usually necessary to establish the diagnosis

- Oral Manifestations may occur weeks or months before the appearance of the skin lesions
- Many patients with oral lichen planus never manifest the cutaneous form of the disease
- Other mucous membranes may be affected also, such as those of the penis, vagina and epiglottis
- The genitals are involved in as many as 25% of women with OLP, compared with only 2–4% of men with OLP.
- Involvement of these locations may occur concomitant with or independent of oral lesions
HISTOPATHOLOGY
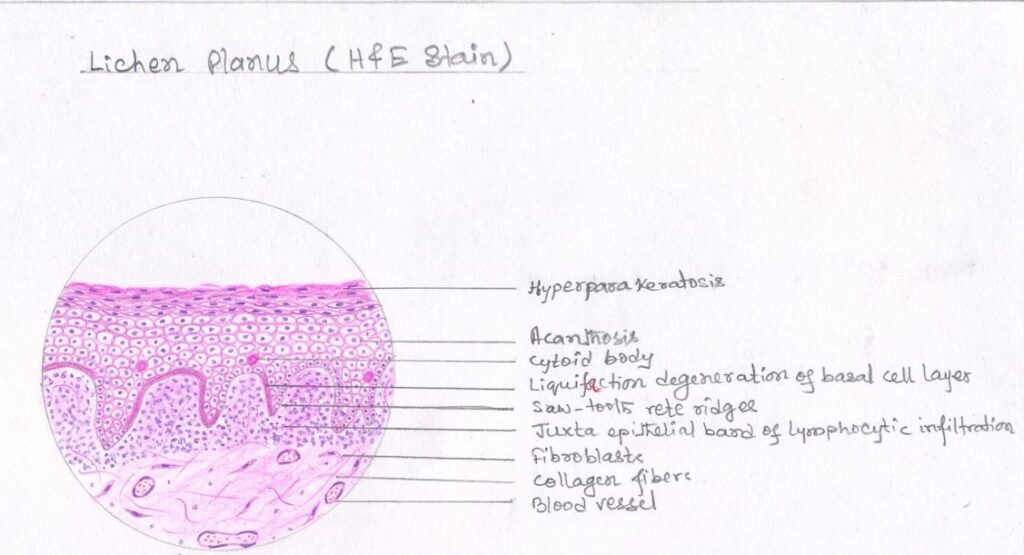
- Typical findings-
- hyperparakeratosis or hyperorthokeratosis with thickening of the granular layer
- acanthosis with intracellular edema of the spinous cells in some instances
- development of a ‘saw tooth’ appearance of the rete pegs
- band-like sub-epithelial mononuclear infiltrate consisting of T-cells and histiocytes
- increased numbers of intraepithelial T-cells
- degenerating basal keratinocytes that form colloid (Civatte, hyaline, cytoid) bodies, which appear as homogenous eosinophilic globules are consistently seen
- Colloid bodies contain fibrin, IgM, C3, C4, and keratin
- Degeneration of the basal keratinocytes and disruption of the anchoring elements of the epithelial basement membrane and basal keratinocytes (e.g. hemidesmosomes, filaments, fibrils) weakens the epithelial-connective tissue interface. As a result, histologic clefts (i.e. Max-Joseph spaces) may form bullae clinically
- The immunopathologic features of lichen planus are nonspecific. Most lesions show the deposition of a shaggy band of fibrinogen at the basement membrane zone.
DIFFERENTIAL DIAGNOSIS
- Leukoplakia
- Candidiasis
- Pemphigus
- Cicatricial Pemphigoid
- Erythema Multiforme
- Syphilis
- Recurrent Aphthae
- Lupus Erythematosus
MALIGNANT POTENTIAL
- Controversy regarding its malignant potential
- slightly higher incidence of oral squamous cell carcinoma in patients with oral lichen planus than in the general population.
- The actual overall frequency of malignant transformation is low, varying between 0.3 and 3%.
- The forms that more commonly undergo malignant transformation are the erosive and atrophic forms
TREATMENT
- At present there is no cure
- long term follow-up recommended
- The principal aims of current OLP therapy are
- the resolution of painful symptoms
- the resolution of oral mucosal lesions
- the reduction of the risk of oral cancer
- the maintenance of good oral hygiene.
- Corticosteroids recommended as its an autoimmune condition (Concern – local and systemic adverse effects and lesion recurrence after treatment is withdrawn)
- Patients should be observed periodically, particularly those with the erosive or atrophic forms and those who also have a history of alcohol and tobacco misuse, because of the risk of malignant transformation
REFERENCES
- Shafer’s Textbook of Oral Pathology – https://amzn.to/3ExQRIW
- Neville Oral & Maxillofacial Pathology – https://amzn.to/3Iu3bvj

